First, Do No Harm
“First, do no harm.” Everyone knows that this is Hippocrates’ famous oath. Every health care worker should live and die by this oath. But how many actually do? It seems to me that the number of those who do is shrinking every day. There are several reasons for this alarming trend.
A. Soaring Economic Overhead. New dentists commonly sport enormous debts. Repayment of debts can become all-consuming. Is it any wonder that so many practitioners see their patients through the lens of economics? They forget that patients are living, breathing human beings who want to be treated with care. Bernard Lown, in his book, The Lost Art of Healing points out that “the moment care is rendered for-profit, it is emptied of genuine caring.” This may not be entirely true, but the trend to view patients as ‘nothing but an assemblage of broken-down biologic parts” seems to be increasing. Patients crave relationship with their doctors and they want doctors who are “sensitive to their aching souls” as much as they are attentive to their “malfunctioning anatomy.” Says Bernard Lown, patients “yearn not for a tautly drafted business contract [complete with consent forms and legalese documents], but for a covenant of trust between equals earned by the doctor while exercising the art of caring.” [Bernard Lown, D: The Lost Art of Healing: Practicing Compassion in Medicine; Ballantine Books (Random House), NY 1996.]
First do no harm means: Put patients first. Treat people the way you would like to be treated. Let go of economic concerns every time you examine a patient and do what is best for them. There will always be patients who need the treatment skills you have to offer.
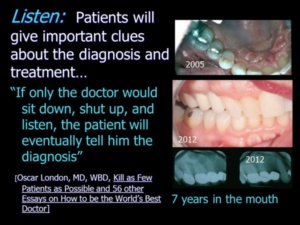 B. No Time to Listen Today, many dentists don’t take the time to actually listen to their patients. Allocating time for listening isn’t considered “productive.” Really? That’s how mistakes begin! “If only the doctor would sit down, shut up, and listen, the patient will eventually tell him the diagnosis;” Oscar London rails. [Oscar London, MD, WBD, Kill as Few Patients as Possible and 56 other Essays on How to be the World’s Best Doctor] With complex cases, taking time to listen can avoid missing important clues to the diagnosis and possible treatment plan. Doctors should see the patient initially in the business office, not the dental chair. In the dental chair, fear can intervene. Enough time must be allocated for the Doctor to listen to the patient’s entire story, clarify the medical and dental history, and establish a rapport. Learning about the patient’s bad dental experience will prevent the doctor from making the same mistakes as the patient’s previous dentist. Attention to listening also communicates that you care—and that elevates the doctor in the patient’s eyes.
B. No Time to Listen Today, many dentists don’t take the time to actually listen to their patients. Allocating time for listening isn’t considered “productive.” Really? That’s how mistakes begin! “If only the doctor would sit down, shut up, and listen, the patient will eventually tell him the diagnosis;” Oscar London rails. [Oscar London, MD, WBD, Kill as Few Patients as Possible and 56 other Essays on How to be the World’s Best Doctor] With complex cases, taking time to listen can avoid missing important clues to the diagnosis and possible treatment plan. Doctors should see the patient initially in the business office, not the dental chair. In the dental chair, fear can intervene. Enough time must be allocated for the Doctor to listen to the patient’s entire story, clarify the medical and dental history, and establish a rapport. Learning about the patient’s bad dental experience will prevent the doctor from making the same mistakes as the patient’s previous dentist. Attention to listening also communicates that you care—and that elevates the doctor in the patient’s eyes.
Once the story has been told, doctors have a unique opportunity to provide general education about Dentistry. Information that takes place before the exam is perceived as education rather than a sales pitch. During this time the Doctor gleans valuable clues about the patient and how receptive to treatment he or she will be when the time comes to present treatment options.
Inadequate listening leads to making snap decisions, which can be disastrous. Trent Hamm, in his essay “The Dangers of Snap Decisions notes that “One of the hardest challenges of modern life is balancing the need to make the right decision with the need to make a fast decision.” [[http://www.thesimpledollar.com/the-dangers-of-snap-decisions/] Trent cautions against doing this: “It is almost always better to get the right answer than to get the quick answer. So often, we apply urgency to something that isn’t urgent and by doing that, we undermine the importance of getting it right.”
Complex cases can be difficult to plan even with a varied toolbox of skills. “Just making the right treatment choice among the many options…can be difficult, even for expert clinicians, ” says the famous physician and author Atul Gawande in his book, The Checklist Manifesto. Often consultation with specialists is needed to help determine the right course of action. I regularly get together with specialists such as orthodontists, endodontists, periodontists, pain management specialists and oral surgeons when I have questions about the direction of treatment. Complex cases may require one or more of these specialties.
It is important that doctors understand that they are treating individuals, not averages. There is no one size fits all when it comes to formulating a treatment plan for a complex case. Often the best treatment involves out-of-the-box thinking. Doctors should take as much time as they need to get it right.
First, do no harm means: Listen to your patients the way you expect them to listen to you. Be an advocate for your patients and seek answers for them that you do not have. Do not arrive at a snap decision because there is only one tool in the shed and it is lucrative to use it.
 C. Inadequate Training: Today, very few dentists have good crown and bridgework skills because these skills are not taught properly. Dentists also don’t understand the corrective value of crown and bridgework in arresting and preventing force-induced degeneration. Unlike fillings or veneers, full coverage restorative dentistry can change architecture and function to prevent tooth loss. However, most dentists are trained to think in a piecemeal way—to fill a hole or a space.” They tend to view crowns solely as “tooth coverings.” Fewer still know anything about precision attachment cases—a treatment option that has the best track record for longevity that can be used with natural teeth or implants. Fixed bridgework that is stretched beyond its limitations is the usual prescription and this approach to care is likely to result in case failure. Patients are much more likely to be harmed with full arch extraction and all-on four implant cases than they are with crown and bridgework and a double-tilt precision attachment case. No one knows how the body will respond to implant therapy, bone grafts and overloading the implants with dental superstructures. The double-tilt precision attachment case, on the other hand, has one of the best track records for longevity and commonly holds up for decades of continuous 24-hour a day wear without replacing the attachments. Sadly, few dental professionals have such a case in their armentarium. Don’t you think they should?
C. Inadequate Training: Today, very few dentists have good crown and bridgework skills because these skills are not taught properly. Dentists also don’t understand the corrective value of crown and bridgework in arresting and preventing force-induced degeneration. Unlike fillings or veneers, full coverage restorative dentistry can change architecture and function to prevent tooth loss. However, most dentists are trained to think in a piecemeal way—to fill a hole or a space.” They tend to view crowns solely as “tooth coverings.” Fewer still know anything about precision attachment cases—a treatment option that has the best track record for longevity that can be used with natural teeth or implants. Fixed bridgework that is stretched beyond its limitations is the usual prescription and this approach to care is likely to result in case failure. Patients are much more likely to be harmed with full arch extraction and all-on four implant cases than they are with crown and bridgework and a double-tilt precision attachment case. No one knows how the body will respond to implant therapy, bone grafts and overloading the implants with dental superstructures. The double-tilt precision attachment case, on the other hand, has one of the best track records for longevity and commonly holds up for decades of continuous 24-hour a day wear without replacing the attachments. Sadly, few dental professionals have such a case in their armentarium. Don’t you think they should?
A high percentage of today’s dentists, however, have great implant skills. As a result, there is an absolute epidemic of tooth extraction and implant placement. Implants are being over-used and used inappropriately. “Often practitioners recommend implants even when teeth are only modestly compromised by caries, the need for endodontic therapy, or periodontal disease to provide the patient with a quick solution to the problem,” say Drs. Giannobile and Lang. “Less trained individuals often recommend tooth extraction rather than retention. This condemns many teeth that could be treated and returned to good function. Even those teeth that are compromised have a much greater life span than the average implant…The long-term prognosis for implants has been shown to be far less promising than that for natural teeth, even when they are compromised by periodontal disease or endodontic problems…”[ Dental Abstracts Vol 61, Issue 4; 2016; Keep the Ones Youve Got; Giannobile, WV, Lang NP: Are dental implants a panacea or should we better strive to save teeth? J Dent Res 95:5-6, 2016]
 It is important to have a complete armamentarium of skills—or the knowledge of where to send the patient for certain skills. If the doctor’s armamentarium includes great skills in crown and bridgework, bonding, precision attachments etc. as well as implants, he or she has the ability to choose which treatment might be best for each patient. But, as Mark Twain and others have said “if all you have is a hammer, everything looks like a nail.” Translation: if all you have are implant skills, every case looks like an implant case. Today there is an absolute epidemic of tooth extraction and implant placement. Implants can be a wonderful option, but too often they are over-used and used inappropriately.
It is important to have a complete armamentarium of skills—or the knowledge of where to send the patient for certain skills. If the doctor’s armamentarium includes great skills in crown and bridgework, bonding, precision attachments etc. as well as implants, he or she has the ability to choose which treatment might be best for each patient. But, as Mark Twain and others have said “if all you have is a hammer, everything looks like a nail.” Translation: if all you have are implant skills, every case looks like an implant case. Today there is an absolute epidemic of tooth extraction and implant placement. Implants can be a wonderful option, but too often they are over-used and used inappropriately.
First, do not harm means: Continuing Education is a must! Seek out qualified individuals to coach you with skills that you do not have or with skills that are weak. Take courses to see what specialists can do for your patients. Learn the pros and cons of each treatment option so that you can make the best recommendations to your patients.
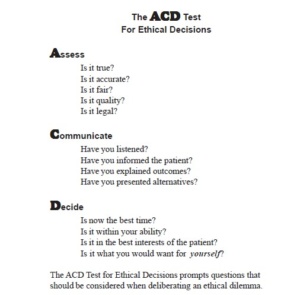
D. The Changing Face of Ethics. The American College of Dentists defines ethics as “the moral principles or virtues that govern the character and conduct of an individual or a group. Ethics, as a branch of both philosophy and theology, is the systematic study of what is right and good with respect to character and conduct.” [Ethics Handbook for Dentists: An Introduction to Ethics, Professionalism, and Ethical Decision Making; American Collage of Dentists; Revised 2016; https://www.dentalethics.org › wp-content › uploads › Ethics_Handbook_for_Dentists_2016.pdf] It is assumed that doctors are steeped with ethics in childhood; that with religious study they are keenly aware of moral precepts and differences between right and wrong. The reality is that cultural norms of ethical precepts can vary considerably.
For this reason, professionals are required to adhere to a professional code of ethics. In 1866, the ADA formally established its Principles of Ethics and Code of Professional Conduct; a rule book that each member is required to live by in order to be called a “professional”. Professionals are held accountable to higher standards than tradesmen because they are required adhere to strict codes of ethics. Under the codes, no professional is allowed to be merely a profiteer. In exchange for the privilege of practice, professionals must be something more. They must be honest, compassionate, straightforward in their relationships, and strive to provide quality care. The Hippocratic Oath is embodied in Section 2 of the ADA Code: “NONMALEFICENCE (“do no harm”). The dentist has a duty to refrain from harming the patient.”
 First, do no harm means: Treat patients the way you would like to be treated. Would you sit for that invasive procedure that you want to perform on patients? Would you like to have choices? Would you like to be eased into major restorative changes instead of drastic treatments like full arch extractions with an immediate denture? “We’ve been wrong about what our job is in [Dentistry], says Atul Gawande in his book Being Mortal. We think our job is to ensure health and survival. But really it is larger than that. It is to enable well-being.”
First, do no harm means: Treat patients the way you would like to be treated. Would you sit for that invasive procedure that you want to perform on patients? Would you like to have choices? Would you like to be eased into major restorative changes instead of drastic treatments like full arch extractions with an immediate denture? “We’ve been wrong about what our job is in [Dentistry], says Atul Gawande in his book Being Mortal. We think our job is to ensure health and survival. But really it is larger than that. It is to enable well-being.”
Harm to the patient can certainly potentially occur from any treatment, and it is rarely caused on purpose. Harm usually arises inadvertently. As Lisa Sanders states in her book Every Patient Tells a Story [2009], “We are regularly wrong in the pursuit of being right.”
Why is there so much hurry to extract teeth? Patients are often told that their teeth are not salvageable when the reality is that other practitioners have the ability to save them. This scenario is common and quite evident in implant presentations and magazine articles. Teeth can always be extracted; and teeth that are not salvageable might be quite useful in supporting interim restorations to ease transitions. Most dentists are not even aware that compromised teeth often tighten up with temporary treatments that change the architecture and the transmission of forces. I have seen miracles! [Take a look at the double-tilt precision attachment case pictured above–that case is such a miracle. It was made on weak roots–short and pointed like nails–on a patient with severe TMJ symptoms. Against all odds it has survived for 30 years with few changes in the X-Rays]. In such a scenario, the prognosis for saving compromised teeth brightens considerably. The dentist has the obligation consider such approaches. The patient has nothing to lose by trying, except a nominal amount of money and time.
I believe strongly that not giving patients choices is unethical. Patients should not be pushed into invasive treatments without providing alternatives. When given choices, most dentists would be surprised at what patients actually choose. Cost is not the only issue; the actual treatment that patients will have to endure is a major consideration. Some patients can’t handle the interim period of wearing an ill-fitting denture while implants are integrating with the bone. These patients might be harmed psychologically as well as physically.
First, do no harm means: understanding the ability of your patient to tolerate treatments. Be kind and provide more care and bedside manner to those who need it. My father always said that people are like horses: some are thoroughbreds, and they have to be handled with kid gloves because they have a very fine-tuned nervous system. And then there is the horse that pulls the milk truck—through the ice, the snow, and the sleet: nothing bothers it.
Become the best practitioner in full coverage restorative dentistry that you can be! Don’t settle! Join the ONWARD program and learn how to do crown and bridgework with excellence and confidence, how to save “hopeless” teeth, and how to provide new options for patient treatment that you never thought of. Visit the website and join here: https://theonwardprogram.com/membership/
Dr. Feinberg is also available to give presentations. His CV and speaker packet is posted on the website. (https://theonwardprogram.com/about-dr-feinberg/) Dr. Feinberg can be reached at info@theONWARDprogram.com.