If all you have is a hammer…
 When it comes to full coverage restorative dentistry, there really is no such thing as “one size fits all.” If you have a variety of tools in your armamentarium, you can pick the right one to fit the job. But, as the saying goes, “If all you have is a hammer, everything looks like a nail.”
When it comes to full coverage restorative dentistry, there really is no such thing as “one size fits all.” If you have a variety of tools in your armamentarium, you can pick the right one to fit the job. But, as the saying goes, “If all you have is a hammer, everything looks like a nail.”
Most dentists really do not have adequate techniques for full coverage restorative dentistry on natural teeth in their armamentarium. How do I know this?
-
Epidemic of Tooth Extraction and Implant Placement: First, teeth that can easily be saved are being extracted in huge numbers in favor of implant placement. This is evident in most dental seminars and journal articles. It is common to see the extraction of teeth flush at the gingiva with excellent roots that can easily support full coverage restorations. These teeth can easily be restored without posts, buildups, fancy extrusion procedures or excessive crown lengthening. In fact, these teeth are fundamentally no different from teeth with clinical crowns, as the ONWARD program clearly demonstrates.
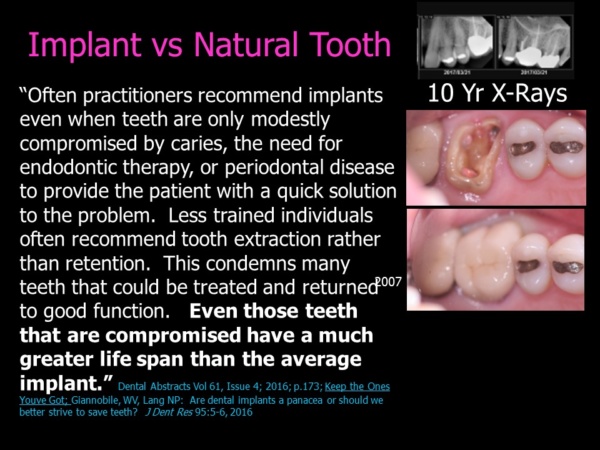 But unfortunately, most practitioners do not know how to save them. Worse, they have zero confidence with crown and bridge techniques in general. No doubt many have had unpleasant experience because the sad truth is that the techniques taught in most dental institutions fall short; and the result is exposed margins, recurrent decay and restorations that fall out.
But unfortunately, most practitioners do not know how to save them. Worse, they have zero confidence with crown and bridge techniques in general. No doubt many have had unpleasant experience because the sad truth is that the techniques taught in most dental institutions fall short; and the result is exposed margins, recurrent decay and restorations that fall out.
At the same time an increasing number of practitioners have excellent implant skills, and they feel much more confident with placing implants than with preparing teeth. All they have is a hammer, so everything looks like a nail. Everyone gets implants instead of saving the natural teeth. This is neither right nor fair.
-
Fear or Preparing Teeth: Second, even renowned presenters appear afraid to prepare teeth! This is apparent in lectures and magazine articles. Often, they prepare teeth for veneers when crowns would be a better option, or they don’t prepare enough teeth to make sound bridgework that has the best prognosis for longevity from an engineering standpoint. Many practitioners cringe at the thought of removing “healthy tooth structure.” What good is preserving tooth structure if the teeth are in jeopardy of being lost altogether? It is truly frightening that so many practitioners today cannot even make a simple six-unit anterior bridge!
-
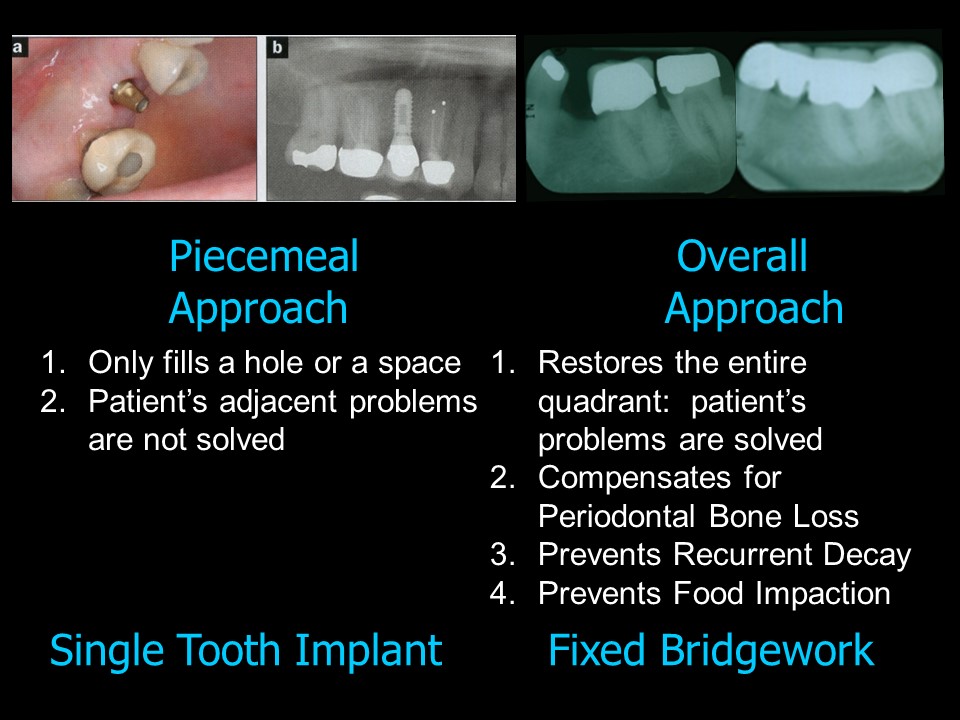
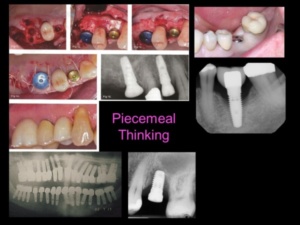
A Piecemeal Approach to Dentistry: Third, most of the single tooth implants are placed among teeth that have crowns or will need crowns in the future. The single tooth implant is the signature of a piecemeal approach to dentistry, and only fills a hole or a space. Single tooth implants are really only indicated where there is no decay or periodontal bone loss on the adjacent teeth.
An overall approach, by contrast, considers the ultimate health and ideal restoration of the whole mouth, or at least a whole area such as a quadrant. When teeth adjacent to a space have large restorations, decay or periodontal bone loss, they are not “virgin” teeth. Bridgework would be a much better option for because the patient’s problems in the entire quadrant would actually be solved. A single tooth implant only fills a hole or a space and does nothing for the adjacent teeth. In this scenario, the patient’s problem is never solved, and the patient ends up with a “hodgepodge.”
-
Viewing Implants as the Solution to All Restorative Problems. Fourth, implants are often stretched beyond their limitations and placed in areas of poor bone quality and depth where they are doomed to failure. Fixtures that have inadequate length, improper angulation, insufficient numbers and incorrect spacing are likely to experience engineering failure after loading the restorations. A patient might be better off with a different strategy than fixed bridgework.
A perfect example is the recent “all-on-four” craze. In many “all-on-four” scenarios, the implants form a clearly deficient foundation for the large superstructures they must support. These superstructures not only replace lost teeth, but lost gingiva and bone as well. Some superstructures do not allow for adequate hygiene around the fixtures. In addition to engineering collapse, failure can also result periodontal problems due to poor hygiene. Once the implants are lost, that patient may not even have the opportunity to place new ones. Usually, bone is lost along with the fixtures. The patient may no longer be a suitable candidate for implants and might even be left with an insufficient ridge to support a denture. Is that really fair?
Renowned expert Carl Misch rails against the overloading of implant fixtures that has become all too common: “The implant practitioner should identify the forces that will be applied to the implant system in formulating a treatment plan. The implant system can be designed to minimize the negative impact of stress on the implant fixtures, the supporting bone, and the final restoration. The design must incorporate strategies to increase implant-bone surface area–such as the use of additional implants, implants of increased width or height, and a decrease in the number of pontics. With these strategies, the retention of the final prosthesis or superstructure is improved, and the incidence of breakage lessened.” [Carl E. Misch, BS, DDS, MDS, PhD (hc); “The Key to Implant Treatment Plans: Stress Treatment Theorem for Implant Dentistry;” Implant Prosthodontics Monographs; Vol. 1, No. 2; June 2017].
-
Failure to Appreciate the Value of Full Coverage Restorations: Most dentists do not understand the real benefits of full coverage restorations. They look at crowns and bridges as mere “tooth coverings.” It is no wonder that they view natural teeth with decay or periodontal bone loss as “unsalvageable” or not worth restoring. Nothing could be further from the truth!
Only full coverage restorations can change the anatomy of the dentition:
-
-
Ideal Shape and Form: Crowns and bridges can be made to an ideal architecture, whereas fillings and veneers only fill a hole or a space. Veneers almost always make teeth bigger than the original teeth because not enough enamel can be removed. In a patient who is susceptible to periodontal bone loss, oversized veneers will overload the foundation and make periodontal problems worse.
-
-
-
Narrower Bucco-Lingual Diameter: Crowns and bridges can be made narrower than the original teeth in order to apply less stress to the periodontal foundation (bone and roots).
-
-
-
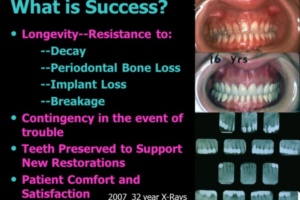
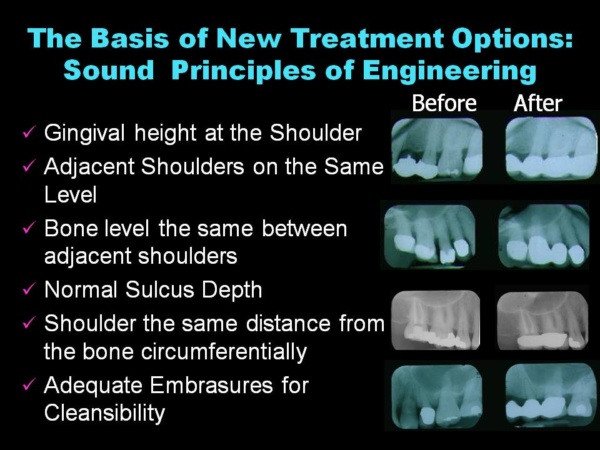
Compensating for Bone Loss to Prevent Future Bone Loss: Crowns and bridges can compensate for periodontal bone loss and bring the forces as close to the bone as possible. When done correctly, the margins of crowns should be close to the bone in the X-Rays. Practitioners have been indoctrinated not to do this for fear of invading biologic width. But 70 years of documented cases shown in the ONWARD program proves otherwise. This practice is not only sound from an engineering standpoint, but also eliminates exposed margins prevents recurrent decay and adds great retentive properties to the restorations.
-
-
-
Splinting (connecting) teeth distributes forces among a group of teeth rather than having each tooth carry the burden of forces individually. Splinting teeth eliminates the possibility of spaces opening between teeth that can cause food impaction areas. Food impaction is a major cause of periodontal bone loss.
-
 Full Coverage Restorations are more predictable on Natural Teeth than on Implant Fixtures. It is important to realize that implants are not panaceas, and they really should be viewed more as feats of engineering than tooth replacements. Unlike roots, implants are cylindrical. When they are placed in the bone no one knows how the tissues are going to heal. It is not unusual to end up with an implant restoration that is an eyesore. Often, crown and bridgework can provide a far more predictable result and is a better choice. Crown and bridgework is far less invasive and can be accomplished much faster than implant restorations. When making full coverage restorations, temporary restorations that are blueprints of the desired result are created immediately. However, it may not be possible to make temporary restorations for implant restorations and the patient might have to walk around with missing teeth while implants osseointegrate for at least 3 months.
Full Coverage Restorations are more predictable on Natural Teeth than on Implant Fixtures. It is important to realize that implants are not panaceas, and they really should be viewed more as feats of engineering than tooth replacements. Unlike roots, implants are cylindrical. When they are placed in the bone no one knows how the tissues are going to heal. It is not unusual to end up with an implant restoration that is an eyesore. Often, crown and bridgework can provide a far more predictable result and is a better choice. Crown and bridgework is far less invasive and can be accomplished much faster than implant restorations. When making full coverage restorations, temporary restorations that are blueprints of the desired result are created immediately. However, it may not be possible to make temporary restorations for implant restorations and the patient might have to walk around with missing teeth while implants osseointegrate for at least 3 months.
 These considerations are extremely important in order to determine the best treatment plan for a patient. If a practitioner has a variety of skills in the armentarium, he or she is able to pick the plan that is best for a particular patient.
These considerations are extremely important in order to determine the best treatment plan for a patient. If a practitioner has a variety of skills in the armentarium, he or she is able to pick the plan that is best for a particular patient.
In treating individuals, there is no such thing as a cookbook solution. Complex restorative problems often require “thinking outside the box” in order to come up with the best corrective plan.
Here are some pointers for choosing the best treatment plan:
-
-
-
Education is key. Learn sound principles and techniques of full coverage restorations or find a referral who excels in this area. Dentistry is a learned profession and continual education is key to becoming the best practitioner you can be.
-
-
-
-
-
Practice Ideal Diagnostic Preparation. Take a full series of periapical X-Rays– panorexes and CBCT scans where needed. Create ideal study models. Take photographs. Write down all your findings on a piece of paper—medical and dental history, dental deformities and pathologies, and the patient’s perceived needs and desires.
-
-
-
Consider all the possibilities. Which choice is least invasive? Which choice has a contingency for that weak abutment, so the entire case doesn’t have to be remade if it fails? Which choice has best chance for longevity? Which plan includes a contingency for that weak abutment? Which case would you want for yourself if you had the same problem? Wouldn’t you rather save your own teeth first?
-
Don’t be afraid to ask for help. Consult with specialists if you have questions or concerns. Often the best treatment involves working with specialists like endodontists, orthodontists, periodontists, and oral surgeons. Take a specialist out to lunch and bring your X-Rays and models.
-
Don’t Make Snap Decisions. You are never obligated to give answers if you are not ready to give them. The first visit in complex cases should be looked at as a “fact-finding mission.” Gather the information and take time to think about it.
If you follow through on these principles, you can successfully “nail” the treatment plan. This makes for a confident doctor and a happy patient. But you might not be using a hammer.
Become the best practitioner in full coverage restorative dentistry that you can be! Don’t settle! Join the ONWARD program and learn how to do crown and bridgework with excellence and confidence, how to save “hopeless” teeth, and how to provide new options for patient treatment that you never thought of. Visit the website and join here: https://theonwardprogram.com/membership/
Dr. Feinberg is also available to give presentations. His CV and speaker packet is posted on the website. (https://theonwardprogram.com/about-dr-feinberg/) Dr. Feinberg can be reached at info@theONWARDprogram.com.